
Research Article
J Pediatri Endocrinol. 2023; 8(1): 1058.
Anesthesia Effect of Remifentanil Combined With Propofol for Elective Small and Medium-Sized Operations in Patients with Uncontrolled Hypertension
Ziye Jia¹; Xiaohan Liu²; Zihan Lei²; Daoqin Gao¹; Ningning Yang¹; Enjun Lei¹*
1Department of Anesthesiology, The First Affiliated Hospital of Nanchang University, Nanchang, PR China
2Department of Medicine, Graduate School, Nanchang University, Nanchang, PR China
*Corresponding author: Enjun Lei Department of Anesthesiology, the First Affiliated Hospital of Nanchang University, Nanchang, PR China. Email: leienjun@126.com
Received: July 13, 2023 Accepted: August 19, 2023 Published: August 26, 2023
Abstract
Objective: To observe the anesthetic effect of remifentanil and propofol in selective small and medium-sized operation for uncontrolled hypertension patients.
Methods: From September 2021 to October 2022, 86 patients with uncontrolled hypertension were selected for elective small and medium-sized operations, including 2 patients with hypertension and coronary heart disease, 15 patients with hypertension and abnormal electrocardiogram, 3 patients with hypertension and diabetes, and 2 patients with hypertension and other systemic diseases. All of them planned to undergo elective small and medium operations (LC in 58 cases, colon cancer in 5 cases, thyroid surgery in 10 cases, intracranial glioma in 7 cases, and total hysterectomy in 6 cases). The operation time was 116±80.6min. Patients with ASA1-4 (66 patients with ASA1-2, 16 patients with ASA3, and 4 patients with ASA4) were aged 28-89 years and weighed 48-98 kg. Propofol 2~3mg/kg, sufentanil 0.4~0.6μg/kg, cisatracurium 0.15~0.2mg/kg were induced intravenously, remifentanil (0.3~0.4μg /kg/min) was pumped, atracurium (1~2μg /kg/min) was pumped to maintain muscle relaxation. Target controlled infusion of propofol with effective chamber concentration of 2 to 5μg/ml, general anesthesia was performed to maintain the minimum effective concentration of sevoflurane combined with inhalation at 0.8 to 1.5 alveolar levels in all patients, and intermittent addition of cisatracurium with 2 to 4 mg to maintain appropriate muscle relaxations. SP, DP, HR, SpO2 were recorded before anesthesia, after induction (A), after tracheal intubation (B), during anesthesia (C), and before tracheal extubation (D). The number of cases of recovery within 5 minutes after the operation, severe hypertension, severe hypotension during anesthesia, and serious complications of hypertension after surgery were recorded.
Results: The induction of anesthesia in this group was basically stable. After induction, the decrease of SP and HR was (36.3±11.8%) and (26.9±11.4%), respectively, which were significantly different from those before induction (P<0.01). SP and HR after tracheal intubation were significantly higher than those after induction (P<0.01), but there was no significant difference compared with those before induction (P>0.05). SP and HR decreased slightly during anesthesia, but there was no significant difference compared with those before induction (P>0.05). The levels of SP and HR before tracheal extubation were significantly higher than those before induction (P<0.01). All patients (100%) were fully awake within 5 minutes after the end of operation. There were 2 cases of severe hypertension and 1 case of severe hypotension during the operation. There were no cases of serious complications of hypertension after the operation.
Conclusion: The application of remifentanil and propofol in the anesthesia of uncontrolled hypertension patients undergoing elective small and medium-sized operations has a definite effect, and the method is simple, safe and reliable.
Introduction
Hypertension is one of the problems that anesthesiologists often encounter, 90%–95% of which are primary and the rest are secondary. In general, treatment for hypertension is recommended in patients with blood pressure above 160/100 mmHg with the aim of reducing it to below 140/90 mmHg [1]. Preoperative treatment and control of hypertension is crucial to reduce the incidence of vascular events during surgery, with a target blood pressure of below 138/83mmHg. As hypertension is a chronic disease, its management forms the foundation for perioperative management of patients with hypertension [2]. The study found that hypertensive patients experienced a 4.9% increase in stroke risk for every 10mmHg increase in systolic blood pressure, and a 4.6% increase in stroke risk for every 5mmHg increase in diastolic blood pressure. Uncontrolled hypertension is a significant risk factor for anesthesia, which in turn poses a substantial risk to both anesthesia and surgery. However, with the advancement of clinical pathways and day surgeries, a significant number of patients with uncontrolled hypertension require elective small to medium-sized surgeries. The administration of anesthesia without antihypertensive treatment based on patient and surgeon preferences has sparked controversy between surgery and anesthesiology department. Propofol is a novel intravenous anesthetic with numerous benefits such as adequate sedation, rapid onset, complete recovery, short clearance half-life, and more. It has the ability to minimize cardiovascular reactions during intubation. Propofol has been found to have additional benefits beyond its sedative properties. It can inhibit the Renin-Angiotensin-Aldosterone System (RAAS), resulting in better inhibition of the stress response. Furthermore, propofol has been shown to stabilize hemodynamics and result in fewer postoperative adverse reactions. In order to address the challenge at hand, we conducted a study from September 2021 to October 2022, with the approval of the hospital's ethics committee. We administered a combination of intravenous remifentanil and propofol to 86 patients with uncontrolled hypertension who were undergoing elective small and medium-sized surgeries. The study yielded satisfactory anesthesia effects. Our findings are summarized as follows:
Materials and Methods
General Information
This study included 86 patients with uncontrolled hypertension, classified as ASA1-4 (66 cases of ASA1-2, 16 cases of ASA3, and 4 cases of ASA4), who were between the ages of 28 to 89 years old and weighed between 48 to 98 kg. Among these patients, there were 2 cases of hypertension and coronary heart disease, 15 cases of hypertension and abnormal electrocardiogram, 3 cases of hypertension and diabetes, and 2 cases of hypertension and other systemic diseases. All patients were scheduled to undergo elective small and medium sized surgeries, including LC in 58 cases, colon cancer in 5 cases, thyroid surgery in 10 cases, intracranial glioma in 7 cases, and total hysterectomy in 6 cases. The average operation time was 116±80.6 minutes.
Methods of Anesthesia
Prior to anesthesia, patients did not receive preoperative medication. Upon entering the operating room, their veins were accessed and they were continuously monitored with ECG and SpO2. An intravenous injection of 2-3 mg/kg propofol, 0.4-0.6 g/kg sufentanil, and 0.15-0.2 mg/kg cis-atracurium was administered for induction. Endotracheal intubation was performed using visual laryngoscopy, followed by the use of the Drager anesthesia machine to regulate breathing. Intermittent Positive Pressure Ventilation (IPPV) was carried out with a tidal volume of 8-10 mL/kg and a frequency of 12 times/min. The suction/exhalation ratio was maintained at 1:2 (I:E). During the operation, PETCO2 was kept at 25-35 mmHg. Patients with ASA3 grade and all patients with ASA4 grade had a three-cavity central venous catheter inserted into their right internal jugular vein under ultrasound guidance to monitor Central Venous Pressure (CVP) and guide fluid replacement. Radial artery placement was performed in ASA4 patients and direct arterial blood pressure was monitored. During the surgery, anesthesia was maintained using a combination of intravenous remifentanil (0.3-0.4μg/kg/min) and atracurium (1-2μg/kg/min) to keep the patient relaxed. Propofol was also administered through a target-controlled infusion, with an effect chamber concentration of 2-5μg/ml. Sevoflurane was intermittently inhaled to maintain the depth of anesthesia at a BIS value of 40-60. The initial infusion rates were 0.2-0.3ug/kg/min for remifentanil and 50-100ug/kg/min for propofol, and were adjusted as needed based on the patient's response to surgical stimulation. The anesthetic infusion was stopped 5 minutes before the end of the operation.
Monitoring and Collection
The patient's spontaneous breathing and oxygen saturation levels were similar to pre-anesthesia levels, and remained above 95% for 5 minutes after sputum aspiration. Once adequate aspiration was achieved, the endotracheal tube was removed. Patients with ASA grades 1-3 were discharged to the ward, while those with ASA grade 4 were transferred to the ICU for further monitoring and treatment. Record the SP, DP, HR, and SpO2 values before anesthesia (N), after induction (A), after intubation (B), during anesthesia (C), and before tracheal extubation (D). The study recorded the number of cases of patients who recovered within 5 minutes after surgery, experienced severe hypertension or severe hypotension during anesthesia, and had severe complications of postoperative hypertension. Additionally, the number of patients who woke up within 5 minutes after the operation was also recorded.
Statistical Processing
The statistical analyses were conducted using SPSS 19.0. The measurement data were presented as mean ± standard deviation (X±S). We used t-test to compare between groups and chi-square test to compare count data. We considered P<0.05 as statistically significant.
Results
The induction of anesthesia in the observed group was relatively smooth. The Systolic Pressure (SP) and Heart Rate (HR) decreased by 36.3±11.8% and 26.9±11.4%, respectively, after induction, which was significantly different from the values before induction (P>0.05). During anesthesia, there was a slight decrease in SP and HR, but not significantly different from values before induction (P>0.05). Before extubation, there was a significant increase in SP and HR compared to before induction (P<0.01). Prior to extubation, both Systolic Pressure (SP) and Heart Rate (HR) exhibited a significant increase, with a notable difference observed from their levels prior to induction (P<0.01). All patients (100%) were fully awake within 5min after operation. There were no cases of severe awareness during operation, 2 cases of severe hypertension and 1 case of severe hypotension, and no case of severe complications of hypertension after operation.
This study examined the experiences of 86 patients with uncontrolled hypertension during operation. Severe fluctuations in circulation, serious complications of hypertension after the operation, awareness during the operation, and recovery within 5 minutes after the operation were all observed and analyzed.
The incidence of severe hypertension during anesthesia and operation was 2.32%, and the incidence of severe hypotension was 1.16%. The full consciousness rate was 100% within 5 minutes after operation.
Discussion
Hypertension is a prevalent disease worldwide, with approximately one in five patients undergoing surgery suffering from it. In the mid-1990s, it was recommended that patients with blood pressure levels above 160/100 mm Hg should receive treatment for hypertension. The goal of this treatment was to reduce the blood pressure levels to less than 140/90 mm Hg. Hypertension is increasingly prevalent in China with about 100 million people affected, accounting for 11.26% of the population. This has led to a rise in non-cardiovascular surgeries amongst hypertensive patients, resulting in a perioperative hypertension incidence of 30%-50%. During induction of general anesthesia, endotracheal intubation can cause hemodynamic instability due to laryngoscope manipulation, endotracheal tube insertion, and pain during intubation, which stimulates the autonomic nervous system, leading to hypertension and tachycardia [3]. Reducing the incidence of perioperative hypertension is crucial in minimizing cardiovascular and cerebrovascular complications during perianesthesia. Anesthesiologists must have a thorough understanding of the pathophysiological changes associated with hypertension during the clearance operation. They should take proactive measures to prevent and treat severe hypertension and hypotension during anesthesia, as doing so can significantly reduce the risk of surgical complications, anesthesia-related issues, and postoperative mortality.
Principles of Elective Surgery for Patients with Hypertension
Hypertensive patients should actively engage in preoperative preparation to improve their tolerance to anesthesia and surgery and reduce the risk of perianesthesia. Ideally, elective surgery should be scheduled after hypertension is controlled, with blood pressure maintained below high normal levels (SP130-139mmHg, DP85-89mmHg). Concurrent diseases should be treated, physiological dysfunction corrected, necessary examinations completed, and vital organ function improved. Additionally, patients should be carefully prepared and their fears and anxieties about anesthesia and surgery should be addressed to reduce the incidence of complications.
Awareness Rate of Patients with Hypertension
The implementation of fast-track and day surgery in hospitals has led to unique scenarios, such as patients being unaware of their hypertension. The awareness, treatment, and control rates of hypertension are crucial factors that impact the treatment and prognosis of the condition. China is a developing country. According to the census results in recent years, the awareness rate, treatment rate and control rate of hypertension in Chinese cities are 36.3%, 17.4% and 4.2%, respectively. In rural areas, it was 13.7 percent, 5.4 percent and 0.9 percent. It is far from the highest awareness rate of hypertension reported abroad (93%-97%). In China, there has been a growing trend towards implementing clinical path, fast channel surgery, and day surgery in recent years. This trend aims to reduce hospitalization time and costs for surgical patients, which has contributed to the low awareness rate of hypertension. In some cases, surgeons are not even aware that their patients have hypertension until blood pressure is detected through continuous monitoring in the operating room during the perioperative period.
Debate on surgery for uncontrolled hypertension patients
According to the principle of anesthesia of hypertensive patients, patients with uncontrolled hypertension should suspend elective surgery. But by this time the patient was already in the operating room and had been prepared for the operation. If the surgery is suspended, it will inevitably be opposed by some patients and their families, and the surgeons are not satisfied with it. It is not conducive to build a harmonious hospital and the public satisfied hospital, and may even cause medical disputes. A study from surgery on whether it is necessary to control blood pressure before abdominal surgery for hypertensive patients shows that pre-operative antihypertensive treatment for grade 1 and grade 2 hypertension does not increase the risk of surgery. In order to ensure the life safety of uncontrolled hypertension patients, anesthesiologists often advocate anesthesia and surgery after regular antihypertensive treatment. Anesthesiologists and surgeons often have heated debates on this issue, which even affect the unity among disciplines.
Anesthetic Management of Patients with Uncontrolled Hypertension
The study of anesthetic methods: It is the inevitable result of medical reform and development that the patients with uncontrolled hypertension undergo elective small and medium-sized surgery. It will become a new research and development direction of anesthesiology to perform anesthesia in hypertension without control treatment before operation. Therefore, it is urgent to study a safe and reliable anesthesia method for patients with uncontrolled hypertension undergoing elective small and medium-sized surgery. In order to solve this anesthesia problem, through animal experiments and clinical studies in our hospital, it was found that remifentanil and propofol intravenous combination can be used successfully for small and medium-sized operation of uncontrolled hypertension patients. The main mechanism is the intravenous combination of remifentanil and propofol, which can achieve a very ideal anesthetic effect, inhibit the circulation itself, and reduce the heart rate and blood pressure to a certain extent. Remifentanil, an opioid receptor agonist, is a new anesthetic drug, which can cause bradycardia, decrease cardiac output, local vasodilation and decrease blood pressure, with a fast effective speed and a short action time [4]. Propofol, as a new intravenous anesthetic, can also inhibit the Renin-Angiotensin-Aldosterone System (RAAS), and the drug metabolism is very rapid, almost no accumulation in the body [5]. When remifentanil and propofol have a good synergistic effect, can achieve good sedative and analgesic effect, can reduce peripheral vascular resistance, can cause a significant reduction in blood pressure and obvious bradycardia [6]. Anesthesia with remifentanil 3ug/L and propofol 2.5mg/L can effectively control blood pressure [7]. Preliminary clinical observation has shown that only that infusion speed of remifentanil and propofol need to be adjusted dure anesthesia surgery, and the systolic blood pressure can be effectively controlled within the range of 90 to 160 mmHg, thereby ensuring the life safety of such patients dure anesthesia surgery, and being an ideal anesthesia method for patients with uncontrolled hypertension [8] addition, the combination of the two methods can not only maintain the stability of intraoperative hemodynamics, but also improve the quality of recovery and reduce complications [9].
Emergency assessment of hypertension before anesthesia: In order to ensure the life safety of patients with uncontrolled hypertension, the anesthesiologist must carry out targeted emergency evaluation. Hypertensive patients are more likely to have hypotensive reactions during anesthesia induction than normal people 10]. Medical, family and social history should be understood as much as possible; Evaluate target organ function and cardiovascular risk factors and comorbidities. Although most of the problems during the perioperative period occur in the undiagnosed and uncontrolled hypertensive patients, as long as the anesthesiologist attaches great importance to it and takes active prevention and treatment for possible risks, the life safety of these patients undergoing surgery can still be well guaranteed.
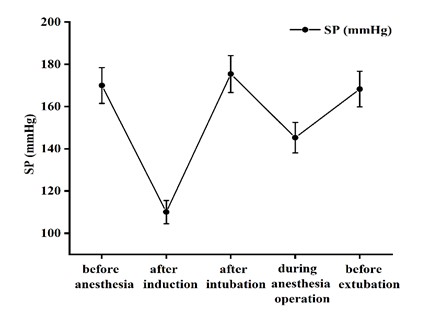
Figure 1: Impact on SP.
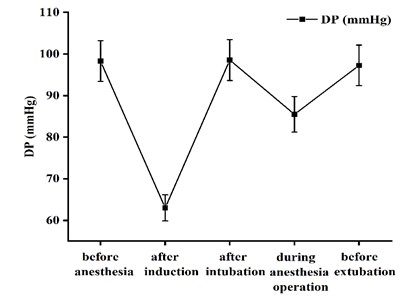
Figure 2: Impact on DP.
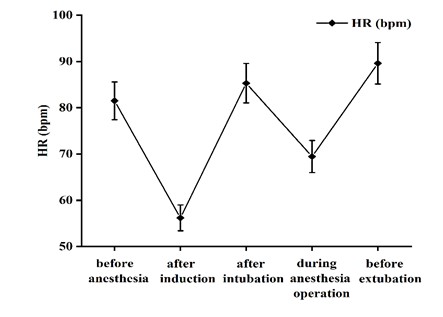
Figure 3: Impact on HR.
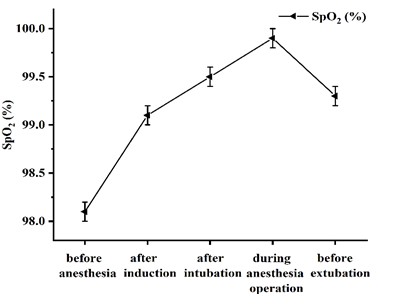
Figure 4: Impact on SPO2.
Establish good circulation monitoring: Blood pressure fluctuates frequently in patients with uncontrolled hypertension during anesthesia. It is very important to strengthen circulation monitoring. This is also closely related to whether the anesthesiologist has clinical experience in treating patients with hypertension [11]. Blood pressure, electrocardiogram and SpO2 should be closely monitored during anesthesia. Non-Invasive Continuous Monitoring (NIBP) is usually used to monitor blood pressure in patients with ASA1-2. When blood pressure fluctuates frequently, especially during induction, endotracheal intubation and extubation, it is recommended to measure blood pressure every 1-2 minutes, and set a high and low blood pressure alarm, so as to attract the attention of anesthesiologists. In ASA4 and some ASA3 patients, direct arterial pressure monitoring and central venous pressure monitoring should be established. PetCO2, Cardiac Output (CO), and Systemic Vascular Resistance (SVR) should be continuously monitored dynamically. Arterial blood gas analysis should be performed when necessary. In order to obtain more hemodynamic parameters data, timely and effective control and treatment.
Careful induction: Serious circulatory accidents can occur during induction of anesthesia in such patients. Laryngoscopy and endotracheal intubation often lead to a sharp increase in blood pressure and heart rate, which can lead to serious consequences for patients at risk of coronary heart disease, heart disease, or cerebral hemorrhage [12]. Intravenous induction with remifentanil and propofol is a good choice. Clinical studies have confirmed that remifentanil can reduce arterial pressure and heart rate by more than 20%. Intravenous remifentanil 1ug/kg and propofol 1-2 mg/kg were given, and only 33% of patients responded to intubation. After induction with remifentanil and propofol, SP and HR decreased significantly in this group (Table 1), which fully indicates that the general condition of patients with uncontrolled hypertension is poor and the cardiovascular compensatory ability is low, which should be paid great attention to by anesthesiologists. Induction dose must be relatively reduced, the speed should be slow. However, the blood pressure and heart rate decreased significantly after induction, which was beneficial to prevent severe hypertension and tachycardia caused by intubation. There is no need to inject esmolol, nicardipine and penehyclidine intravenously before tracheal intubation to prevent the stress reaction of intubation. In this group, blood pressure and heart rate increased significantly 1–2 min after intubation as compared with those after induction (SP increase >35%, P<0.01); The increase in HR was greater than 20%, P<0.01), but it was not significantly different from that before induction (increase <10%, P>0.05). The incidence of severe circulatory fluctuation during the perioperative period was low in this group (3.48%), and no cerebrovascular or cardiovascular accident was reported. The main reason was that blood pressure was effectively controlled in all stages of anesthesia (Table 2).
N
A
B
C
D
SP (mmHg)
170±14.17
110±13.28**
175.4±13.87
145.27±11.56
168.23±15.38
DP (mmHg)
98.3±13.67
63.±12.17**
98.54±12.37
85.48±11.24
97.26±15.73
HR (bpm)
81.5±12.3
56.2±9.68**
85.3±16.5
69.46±11.8
89.6±11.8
SpO2 (%)
98.1±0.5
99.1±0.3
99.5±0.5
99.9±0.1
99.3±0.6
Compared with before induction, △P<0.01 after induction, △P<0.01 after induction, but △P> .05 before induction. There was no significant change in SpO2 at each stage P>0.05.
Table 1: Changes of SP, DP, HR and SpO2 before anesthesia,(N) after induction (A), after intubation (B), during anesthesia operation (C), before extubation (D).
Severe hypertension
Severe hypotension
Severe knowledge in within 5 minutes
Postoperative operation
Complications recovery
86 Examples
2
1
0
0
86
Table 2:
Principle of blood pressure regulation in anesthesia surgery: During anesthesia, we should hold the concept of overall situation and integrity, closely cooperate anesthesia with surgery, give priority to prevention, strengthen intraoperative monitoring, maintain proper anesthesia depth, effectively control blood pressure, ensure patient safety, and achieve successful surgical treatment. Regardless of the rise or fall in blood pressure, as long as it is not more than 20% of the original blood pressure, the perfusion of various important organs and tissues is good, all of them are within the scope of compensation, and there is no such manifestation as ischemia and hypoxia [13-15]. Hypertensive patients with uncontrolled treatment, blood pressure fluctuation during anesthesia is almost unavoidable, but the range of blood pressure fluctuation should be about 110~150/70~100mmHg. An increase or decrease in blood pressure beyond physiological limits can lead to serious complications such as stroke, cerebral hypoxia, myocardial ischemia, myocardial infarction, heart failure, renal failure, and respiratory failure, and even death. Therefore, how to maintain the patient's blood pressure is relatively stable during anesthesia, and how to regulate the blood pressure within the physiological permissible range is the key to anesthesia management.
Control of blood pressure during anesthesia: The main reason for high blood pressure during anesthesia operation is light anesthesia. There is no perfect objective index to monitor the depth of anesthesia in clinic, so the depth of anesthesia can only be judged by clinical manifestations. Intravenous infusion of 0.0008% remifentanil and 0.14% propofol can quickly deepen anesthesia and effectively control blood pressure. When the blood pressure is too high, we only need to increase the infusion speed to control the blood pressure to a reasonable level. It is necessary to prevent the occurrence of hypotension while keeping watch for the occurrence of severe hypertension in patients with uncontrolled hypertension during anesthesia. Such patients due to neurological, mental, body fluid, endocrine dysfunction and other factors, leading to small artery spasm, vascular wall hardening, vascular cavity narrowing and blood concentration, sustained intraoperative hypotension, will cause serious complications, such as myocardial infarction, cerebral thrombosis and renal hypoperfusion [16]. When the blood pressure is too low, stop or slow down the infusion of anesthetic drugs, and the blood pressure can rise to the ideal range after 3 to 5 minutes. Because remifentanil and propofol are metabolized very rapidly in the body, they will lose their antihypertensive effect in a short time. When the above treatment is not effective, vasopressors are considered, and 4mg of dopamine is commonly given intravenously. In addition, when hypotension is treated, blood volume should be supplemented in time to correct electrolyte and acid-base disorders.
Strengthen the management of anesthesia recovery period: On recovery from anesthesia, due to wound pain, tracheal tube stimulation, sputum aspiration, cough, and tracheal tube removal, the blood pressure of uncontrolled hypertensive patients can easily rebound seriously, which is a high incidence stage of anesthesia accidents. At the end of surgery and when the endotracheal tube is removed, in case of severe hypertension, rapid infusion of anesthetic drugs or single or intravenous propofol can be used to control blood pressure. Remifentanil and propofol have obvious advantages compared with traditional anesthesia in patients with uncontrolled hypertension during elective surgery. Remifentanil and propofol are metabolized quickly in vivo, and patients can wake up after 5 mins to 10 mins of drug withdrawal, avoiding the increase in blood pressure caused by the use of opioid antagonists. The patient can tolerate endotracheal intubation well after recovery, and there is no disturbance during recovery period, which is conducive to the stability of circulation. After extubation, the patient can follow the anesthesiologist's guidance, which is conducive to the patient's own clearance of respiratory secretions, and avoid severe hypertension caused by adverse stimulation such as sputum aspiration.
Strengthen the management of tracheal extubation: For severe hypertension after extubation, intravenous injection of nitroglycerin, nicardipine, urapidil, Esmolol and other short-acting antihypertensive drugs can be used for control. After extubation, the mask of anesthesia machine should be used to supply oxygen to prevent hypertension caused by hypoxia and carbon dioxide retention. Patients with ASA4 should be admitted to ICU for further observation and treatment. In addition, the rapid removal of remifentanil may lead to insufficient postoperative analgesia. It is necessary to give postoperative analgesia in time to reduce severe hypertension caused by pain stimulation.
Conclusion
Maintaining the stability of hemodynamics, ensuring the blood perfusion of tissues and organs, avoiding the drastic fluctuation of blood pressure and preventing the complications caused by low or high blood pressure are the key points of anesthesia for uncontrolled hypertension patients. Remifentanil and propofol used in the anesthesia of uncontrolled hypertension patients are simple, safe, easy to master and implement. The blood pressure drops smoothly during blood pressure control, and there is no drug tolerance or regression phenomenon. Compared with other antihypertensive drugs, it has little physiological interference to patients, and can achieve good general anesthesia effect and effectively implement controlled antihypertensive. It provides a safe and reliable anesthesia method for patients with uncontrolled hypertension, reduces the hospitalization time and total hospitalization cost for patients with uncontrolled hypertension, and helps to solve the practical problems of difficult and expensive hospitalization for the masses.
References
- Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C et al. ACC/AHA/AAPA/ABC/ACPM/AGS. Hypertension. 2018; 71: e13-e115.
- Foëx P, Sear JW. Implications for perioperative practice of changes in guidelines on the management of hypertension: challenges and opportunities. Br J Anaesth. 2021; 127: 335-40.
- Lee SK, Jeong MA, Sung JM, Yeon HJ, Chang JH, Lim H. Effect of remifentanil infusion on the hemodynamic response during induction of anesthesia in hypertensive and normotensive patients: a prospective observational study. J Int Med Res. 2019; 47: 6254-67.
- Tao M. Effect of propofol combined with remifentanil in elderly patients with hypertension. Chin Mod Doct. 2016; 54: 132-4.
- Effect of propofol combined with remifentanil on surgical anesthesia in elderly patients with hypertension. Chin J Gerontol. 2011; 31: 2850-1.
- Gong H. Effects of different anesthetic drugs on stress response in elderly patients undergoing laparoscopic cholecystectomy. Chin Mod Doctors. 2013; 51: 109-11.
- Pan T, Lei Y, Lei Z, Lei Z, Fang Y, Xu R et al. Clinical study on anesthesia with remifentanil and propofol in patients with high hemodynamics. Altern Ther Health Med. 2022; 28: 44-9.
- López Castilla JD, Sánchez Fernández N, Charlo Molina MT, Vázquez Florido A, Murillo Pozo MA, Sánchez Ganfornina I, et al. Midazolam/fentanyl vs propofol/remifentanil in immediate postoperative with short-term mechanical ventilation. Ann Pédiatr. Engl ed. 2022; S1695-4033: 30516-6.
- Cui H, Min S. Effects of propofol combined with remifentanil on anaesthesia in elderly patients with hypertension. Chin J Gerontol. 2013; 33: 1744-6.
- Hojo T, Kimura Y, Shibuya M, Fujisawa T. Predictors of hypotension during anesthesia induction in patients with hypertension on medication: a retrospective observational study. BMC Anesthesiol. 2022; 22: 343.
- Zhang H. Discussion on surgical anesthesia and measures to prevent blood pressure fluctuation in patients with hypertension. Chinese medicine guidelines. 2011; 9: 472-3.
- Vickovic S, Zdravkovic R, Radovanovic D, Galambos IF, Pap D, Krtinic D et al. Effect of different doses of remifentanil on the cardiovascular response after endotracheal intubation: a randomized double-blind study. Eur Rev Med Pharmacol Sci. 2023; 27: 653-8.
- Salmasi V, Maheshwari K, Yang D, Mascha EJ, Singh A, Sessler DI, et al. Relationship between intraoperative Hypotension, Defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology. 2017; 126: 47-65.
- Charlson ME, MacKenzie CR, Gold JP, Ales KL, Topkins M, Shires GT. Intraoperative blood pressure. What patterns identify patients at risk for postoperative complications? Ann Surg. 1990; 212: 567-80.
- Goldman L, Caldera DL. Risks of general anesthesia and elective ope¬ration in the hypertensive patient. Anesthesiology. 1979; 50: 285-92.
- Xianling T, Chunyan W, Zhuhua L. Clinical study on the effect of general anesthesia on blood rheology of hypertension patients during perianaesthesia. Chin J Hemorheol. 2006; 01: 61-3.