Abstract
Background: The underlying bone framework always determines the soft tissue contours. Numerous aetiologies are linked to tooth loss, which frequently causes abnormalities of the alveolar ridge. Alveolar bone changes in volume as a result of physiologic bone remodelling after tooth extraction, which impacts the way how edentulous area is treated with prosthetic rehabilitation. By limiting the natural post-extraction resorption process, socket preservation methods following tooth extraction will lessen the need for additional ridge augmentation techniques before implant placement while maintaining the existing bone.
Case Report: Two male patients, ages 36 and 32, were referred for the extraction of their severely deteriorated first molars in the mandible and for the placement of dental implants to restore the area. Patients were identified as having periodontitis and root caries respectively. In one example, the socket was promptly grafted with Platelet Rich Fibrin with xenograft, and in the other with a collagen sponge, after the irreparable tooth was “atraumatically” excised without creating a flap. After suturing the region, a periodontal dressing was applied and no membrane was employed.
Conclusion: After six months, the ridge’s architecture was preserved, and clinical examination showed outstanding soft tissue healing. At six months, a clinical and radiological follow-up evaluation demonstrated consistent and positive outcomes. This article discusses and emphasises the significance of socket preservation after tooth extraction utilising different biomaterials in different case scenarios.
Keywords: Socket preservation; Ridge preservation; Resorption; Implants
Introduction
Following tooth extraction, volumetric changes in the remaining ridge are expected [1]. Difficult tooth extraction procedures can result in further bone loss due to surgical trauma [1]. According to Botticelli et al. study, buccal bone resorption is more severe than lingual bone resorption. By preserving the alveolar ridges after the tooth is removed, it facilitates the eventual placement of implants. Since it supports healthy keratinized tissue and sets the soft tissue profile, which reflects the underlying bone form, alveolar bone is crucial for long-term cosmetic success [1].
Socket preservation is a suitable remedy for the low bone volume as well as rapid bone loss following tooth extraction [2]. "In an approach known as "socket preservation," bone grafts materials are placed in the socket at the time of tooth extraction [2]." There are several bone graft materials, including autologous grafts, allogenic materials, and xenografts, that can be used to preserve extraction sockets [3]. These bio-materials in the extraction socket mainly act as volume preservers and space makers, and they generated a relatively little change in the extraction socket. However, the materials choose depends on how the socket will be preserved [3].
Here, we show two distinct cases of socket preservation employing Platelet Rich Fibrin (PRF) with xenograft and collagen plugs. These cases were done in view of the significance of hard and soft tissue healing at extraction sites as well as investigations of the role of various bio-materials for the same.
CASE 1: Socket Preservation Using Platelet Rich Fibrin (PRF) and Bone Grafts
Clinical History and Management
A 36 year old male patient who visited the department of periodontics with a chief complaint of mobile teeth with mandibularr right back tooth region. The patient's medical history was normal, and no drugs were being taken by him. Oral clinical examination reveals grade 3 mobility with mandibular right first molar (Figure 1A). The Intra Oral Perapical (IOPA) Radiograph showed there is no bone support with mandibular right first molar (Figure 1B). After discussing the treatment options with the patient, he agreed for extraction of the teeth, followed by socket preservation with bone regeneration for implant placement. From the patient informed written consent was obtained. Two weeks before the surgery, a thorough scaling and root planing was carried out. 9 ml each of venous blood samples were taken prior to extraction on the day of procedure. The PRF manufacturing procedure was strictly followed when the blood samples were taken. Using a specific centrifuge, the Hettich® Universal 320, the venous blood was immediately centrifuged at 400xg at room temperature for 10 min. It was then set aside for 3-5 min. Red Blood Cell (RBC) debris was placed at the bottom layer, PRF gel was placed in the middle, and supernatant was placed at the top layer (Figure 1C). During surgery, under local anaesthesia a periotome was utilized to separate the periodontal fibers and subsequently luxate the tooth. After that, extraction forceps were used to remove the tooth. (Figure 1D) Following extraction, the residual granulation tissue was removed by curettage in the socket using a spoon excavator and saline irrigation was done (Figure 1E). The RBC layer was removed from the PRF gel using sterile tweezers. After saline irrigation, PRF membranes were cut to the appropriate size, mixed with (CERABONE PLUS) bone graft, and implanted (Figure 1F) into the extraction socket (Figure 1G). Following suturing (Figure 1H) and periodontal pack placement, the patient was given post-operative instructions and medications to reduce the risk of infection. The patient was given the prescriptions for 500 mg of amoxicillin TDS for 5 days and 400 mg of metronidazole TDS for 5 days. In order to lessen the patient's postoperative pain, paracetamol was administered. The sutures were removed after a week. The patient was recalled for a clinical and radiological assessment after six months. Six months from the procedure, the patient was reevaluated for implant placement. Clinical assessment of the socket preservation location revealed that the tissues had healed properly (Figure 1I) and radiographic analysis revealed radiopacity at the grafted site, indicating bone regeneration at the socket preservation area (Figure 1J).

Figure 1A: Probing pocket depth 15 mm.
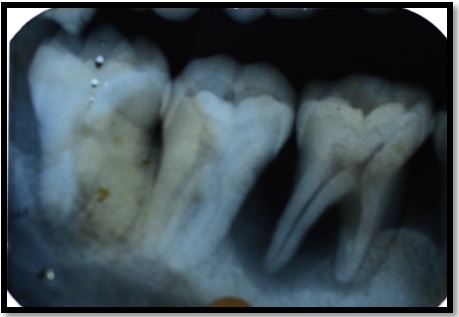
Figure 1B: Pre operative IOPA.

Figure 1C: PRF.

Figure 1D: Extraction irt 46.
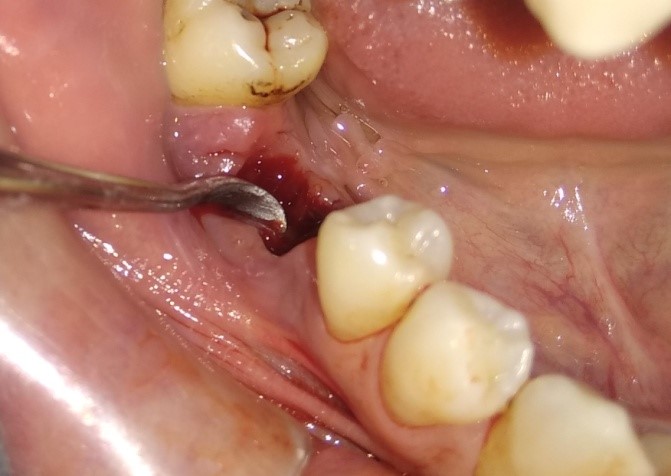
Figure 1E: Curetting the socket.
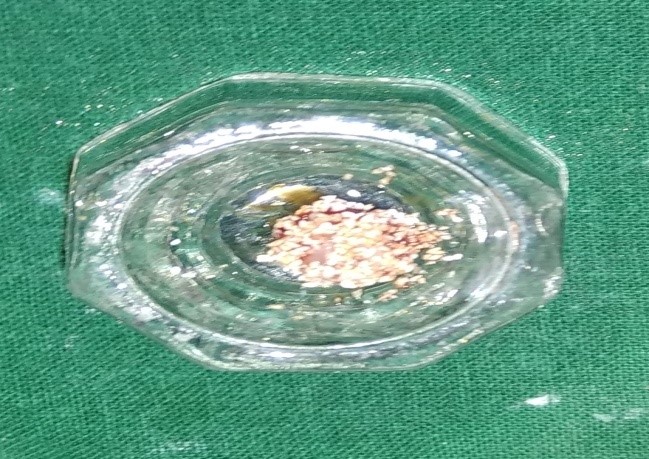
Figure 1F: PRF + CERABONE.

Figure 1G: Graft placed with socket.

Figure 1H: Sutures placed.

Figure 1I: months post operative view.
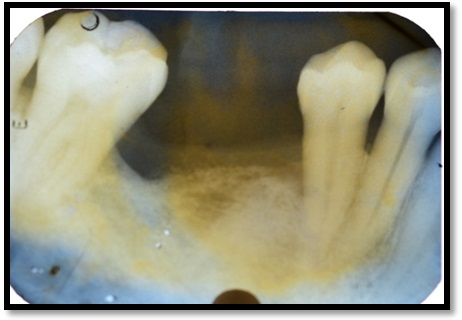
Figure 1J: 6 months post operative IOPA.
CASE 2: Socket Preservation Using Collagen Plug
Clinical History and Management
A 32-year-old male with a non-contributory medical history, presented to our department with a grossly decayed tooth lower right back tooth region. During an intraoral clinical examination, the right mandibular first molar was found to have carious root stumps (Figure 2A). A periapical radiograph examination of tooth number 46 demonstrated an apical resorption (Figure 2B). After being determined to be beyond saving, the tooth was recommended for extraction with socket preservation for potential dental implant placement.

Figure 2A: Root stump irt 47.

Figure 2B: Pre operative IOPA.
The written informed consent was obtained from the patient before the treatment was scheduled and performed. The tooth was removed using an atraumatic extraction approach and a Periotome instrument to preserve the crestal bone (Figures 2C). A collagen plug (DSI COLLAGEN PLUG) was grafted after manual curettage of the extraction site to remove granulation tissue and saline irrigation (Figures 2D-2F). Without making a periosteal release incision, the wound was sutured up with non-absorbable suture (Figures 2G) followed by periodontal dressing. Analgesic-anti-inflammatory, Dolonex DT (Piroxicam 20 mg) twice daily for 3-5 days and a antibiotic, Augmentin 625mg (Amoxycillin 500mg + Clavulanic acid 125 mg), were prescribed. After a week, the sutures were removed and healing was satisfactory. At the grafted site, both excellent aesthetics and a pleasing soft tissue contour were maintained. After six months, the patient was recalled for evaluation and scheduled for prosthetic rehabilitation (Figure 2H, 2I).

Figure 2C: Extraction irt 47.

Figure 2D: Curetting the scoket.

Figure 2E: Collagen sponge plug.

Figure 2F: Sponge placed with socket.

Figure 2G: Sutures placed.

Figure 2H: 6 months post operative.

Figure 2I: 6 months post operative IOPA.
Discussion
After a tooth is extracted, an approach called socket preservation is used to reduce the loss of alveolar bone [2]. This surgery usually involves filling the tooth socket with biologic agents, bone graft material, or barrier membrane as soon as the tooth has been extracted [3]. Even when done carefully and in a atraumatic manner, tooth extraction will result in changes to the alveolar bone's dimensions on both a horizontal and vertical axis. As a result, it will be difficult for dentists to replace missing teeth with dental implants or any other type of prosthesis [4]. In the first six to twelve months after tooth extraction, this bone loss occurs very quickly. According to research, socket preservation of extraction sockets can be a treatment option for reducing post operative resorption [2].
The socket seal surgical approach and the Bio-Col technique are two methods that have evolved over time to solve the flap advancement limitations [5]. "Some publications refer to the different socket preservation strategies as "socket plug" methods. The four steps of this surgery include atraumatic tooth extractions, a conservative flap design, the implantation of acceptable biomaterials, and suturing [6].
The alveolar ridge can be preserved utilizing a variety of techniques and procedures, including regenerative treatments using autografts, allografts, and xenografts with or without a collagen plug, resorbable/non-resorbable membranes, immediate implants, and the use of PRF [3]. Then, to avoid the material loss, these components can be covered with a membrane or autologous tissue [3]. The alveolar bone can be preserved using these materials, which have demonstrated favourable results [6]. The bio material used in this case reports are PRF with xenograft and collagen plug. A novel method for preserving the extraction socket is the use of a collagen plug, a cylinder-shaped collagen sponge [6]. This substance acts as a scaffold in the extraction socket and a chemotactic substance for fibroblasts [6]. Furthermore, it aids in the hemostasis of the extraction site [6]. Over the past ten years, there have been multiple improvements made to the "socket plug technique," which entails employing different mixes of collagen and bone graft materials [6]. Regarding the preservation of alveolar bone, this procedure has shown to be consistent and to produce predictable results [6].
Another study conducted by Araujo and published in 2009 showed that adding biomaterial to an extraction socket can improve bone modelling and account for marginal ridge contraction [7]. The interproximal bone between the tooth and the implant was preserved, as demonstrated in the current clinical case, and the socket preservation procedure produced successful aesthetic results, including the lack of the grey hue in the free gingiva. A narrow neck implant could be placed in the best location due to the preserved bone's size, and the occlusal forces that resulted did not overload the patient or compromise their prognosis. It has been noted that the mandible exhibits more ridge resorption than the maxilla [8]. There have been numerous studies comparing the BIC (Bone Implant Contact) of natural bone to regenerated bone. According to Trisi, BIC in implants with rough surfaces can improve by up to 72% over time [9]. The BIC at areas grafted with bovine bone grafts is higher than in the nongrafted sites, according to a study by Valentini [10]. The purpose of this paper is to emphasize the rationale for maintaining the dimensions of the extraction sockets. PRF is made from venous blood and exhibits a three-dimensional, flexible, and long-lasting network structure. Fibrin, platelets, white blood cells, growth factors, cytokines, and other elements helpful for tissue healing are abundant in PRF [11]. Considering the organisational and biological traits, PRF is a safer, more efficient, and more cost-effective transplant material for preserving the alveolar site [12]. In socket preservation treatments, xenografts are thought to be the most often utilised bone fillers because of their osteoconductive qualities, which encourage the formation of new bone surrounding them [11].
In conclusion, it was shown that the PRF utilised in the extraction sockets promoted local soft tissue healing of the gums and decreased postoperative pain response [12]. The concentration of growth factors in PRF allowed it to improve the quality of the novel bone and the rate of bone development [11].
Conclusion
Since the collapse of hard and soft tissues is usually triggered by tooth loss due to caries or trauma, bone volume preservation is essential for ensuring proper implant and aesthetic rehabilitation. For implant therapy to be effective there must be a significant amount of healthy bone at the recipient site at the time the implant is inserted. Currently, introducing bone graft material into the extraction socket, covering it with a cross- or non-cross-linked membrane, and then securing the flap is the most typical procedure for ridge preservation. It is up to each person whether or not to use the socket preservation strategy. Surgeons must be aware about the wide range of procedures and biomaterials used in order to improve preserve the hard and soft tissue forms. When using the socket preservation approach in their regular practice, physicians can get knowledge from this article that will be helpful. In order to get the most functional and aesthetically pleasing prosthesis after implant rehabilitation, the socket preservation procedure appears to produce significant outcomes regarding bone volume conservation and favourable architecture of the alveolar ridge. Similar clinical situations, particularly in the maxillary and mandibular front regions, are frequently found after dental treatment when the thin labial cortical bone resorbs postextraction. Such a sequel could be problematic for dental implants. In order to prevent bone resorption and attempt to restore and maintain bone through socket preservation techniques, it is crucial for every dental professional to forecast the post-extraction healing outcome.
Author Statements
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given his consent for his images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
References
- Botticelli D, Berglundh T, Lindhe J. Hard tissue alterations following immediate implant placement in extraction sites. J Clin Periodontol. 2004; 31: 820-8.
- Wang HL, Kiyonobu K, Neiva RF. Socket augmentation: rationale and technique. Implant Dent. 2004; 13: 286-96.
- Kim YK, Yun PY, Lee HJ, Ahn JY, Kim SG. Ridge preservation of the molar extraction socket using collagen sponge and xenogeneic bone grafts. Implant Dent. 2011; 20: 267-72.
- Alani AF. Multiple techniques have been proposed to preserve alveolar bone after tooth loss. Ann Med Health Sci Res. 2018; 8: 65-8.
- Coomes AM, Mealey BL, Huynh-Ba G, Barboza-Arguello C, Moore WS, Cochran DL. Buccal bone formation after flapless extraction: A randomized, controlled clinical trial comparing recombinant human bone morphogenetic protein 2/absorbable collagen carrier and collagen sponge alone. J Periodontol. 2014; 85: 525-35.
- Sun Y, Wang C, Wang Z, Cui Y, Qiu Z, Song T, et al. Test in canine extraction site preservations by using mineralized collagen plug with or without membrane. J Biomater Appl. 2016; 30: 1285-99.
- Araújo MG, Lindhe J. Ridge alterations following tooth extraction with and without flap elevation: an experimental study in the dog. Clin Oral Implants Res. 2009; 20: 545-9.
- Irinakis T. Rationale for socket preservation after extraction of a single-rooted tooth when planning for future implant placement. J Can Dent Assoc. 2006; 72: 917-22.
- Lekovic V, Camargo PM, Klokkevold PR, Weinlaender M, Kenney EB, Dimitrijevic B, et al. Preservation of alveolar bone in extraction sockets using bioabsorbable membranes. J Periodontol. 1998; 69: 1044-9.
- Valentini P, Abensur D, Densari D, Graziani JN, Hämmerle C. Histological evaluation of Bio-Oss in a 2-stage sinus floor elevation and implantation procedure. A human case report. Clin Oral Implants Res. 1998; 9: 59-64.
- Simon BI, Zatcoff AL, Kong JJ, O’Connell SM. Clinical and histological comparison of extraction socket healing following the use of autologous Platelet-Rich Fibrin Matrix (PRFM) to ridge preservation procedures employing demineralized freeze dried bone allograft material and membrane. Open Dent J. 2009; 3: 92-9.
- Del Fabbro M, Bortolin M, Taschieri S. Is autologous platelet concentrate beneficial for post-extraction socket healing? A systematic review. Int J Oral Maxillofac Surg. 2011; 40: 891-900.
- Barone A, Todisco M, Ludovichetti M, Gualini F, Aggstaller H, Torrés-Lagares D, et al. A prospective, randomized, controlled, multicenter evaluation of extraction socket preservation comparing two bovine xenografts: clinical and histologic outcomes. Int J Periodontics Restorative Dent. 2013; 33: 795-802.
